Progress is defined by Merriam Webster as ‘a forward or onward movement (as to an objective or to a goal)’. In reflecting on my #MHST601 learning journey, I feel that I have achieved progress. This is my first foray into graduate studies, and it is taking place many years after my undergraduate studies. To say I felt rusty is a gross understatement. Added to that, I am approaching graduate school at a busy time in my life with a fairly new job, busy work and personal life and many other time commitments. This has impacted my ability to focus solely on the course and to give it my undivided attention. Alongside my learning about our health systems and the challenges faced by many in accessing the services and supports they need to be healthy, I have also personally learned how I can best succeed in distance learning and being in school at this point in my life. I have learned that I need to carve out specific evenings to complete my school work and I cannot waver in this or I will get behind. I also need to chunk out the weeks requirements and prioritize what I can achieve on my study nights to ensure I can meet the requirements of the week. I needed to find the balance.
The content that we have covered in #MHST601 has also been a progression for me to learn more about health care in Canada and this has inspired me to better use my role in the system to be a change maker. We began with some reflection on our personal social media presence(s) and some discussion about the intersection between personal and professional personas on social media platforms. This was something I have been aware of certainly but had not critically assessed my own presence before. We also began our resource curation journey. From here we were tasked to create an e-portfolio and to consider our role in health care as it relates to Federal and Provincial roles and mandates. I vividly recall when initially being asked to create an e-portfolio feeling very apprehensive about this assignment/project. I am not super techie and did not know where to begin. I also did not see initially how this would be helpful for my learning or growth. I struggled quite a bit with it but was able to create something that I am happy with. I do see the importance of curating resources/thoughts and topics related to the course in this way now, especially as I have been able to look back on them and see the growth and progress. I will not be seeking a career change to be a web developer anytime soon – I still feel rusty and not super confident when updating my e-portfolio, but I will keep the e-portfolio going throughout my MHS journey and I am much more confident in my abilities now than in Unit 2.
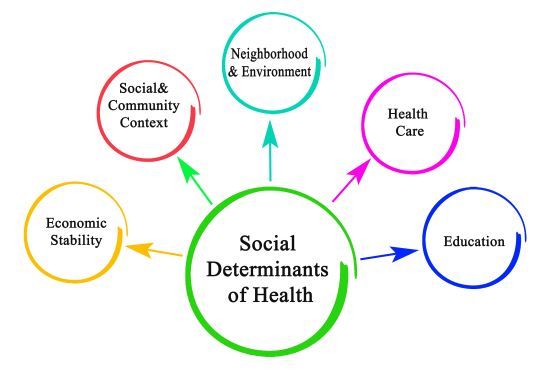
From here we began to look at health determinants and to start our journey to better understand that all is not even nor fair when it comes to health outcomes. As a public health nurse, social determinants of health (SDOH) are not new to me, but I benefitted from learning more about SDOH and their impact on health in this unit. Modifiable SDOH are very difficult to positively impact in the current siloed state of our health care and social systems. I chose to post about the impact that 2SLGBTQIA+ stigma has on health outcomes for folks who are part of this community. This is a topic of importance to me personally and in the sexual health clinics in which I work.
I also introduced the topic of proportionate universalism in one of my posts, which is something that I have been studying as it relates to the services we offer in my clinics – proportionate universalism is understanding that some individuals will need more comprehensive services to meet their needs as compared to others to achieve the same health outcomes. This is an important consideration when planning for the delivery or evaluation of health services. I also referred to the Basic Income Pilot that was implemented in Ontario and subsequently cancelled in 2019 by the incoming government without finishing it nor evaluating it. This is such a shame as the preliminary data was very positive. The negativity surrounding the concept was fierce by some groups in Ontario who felt that this was a money handout and not a good use of taxpayers dollars. However, the data derived from the pilot showed that families who qualified for the basic income supplement (those living below the basic income threshold) were able to use this supplement to ‘level up’ and then be able to enroll kids in sports, gain purchasing power, start small businesses, etc. The evaluation data collected showed very positive impacts in physical health, mental health, and well-being for both participants and others in their households. Also, 71% of respondents reported feeling less tired and 57% reported less physical pain. Recipients also reported less use of tobacco (56%) and alcohol (48%). They were less stressed (86%), less likely to be depressed (83%), and had a more positive outlook on life (86%). This contributed to fewer demands on the public health system (Ferdosi et al, 2022).
Next we embarked on better understanding existing multilevel health models as a means to position the many factors that impact health within a systems approach. I worked with the social ecological model.
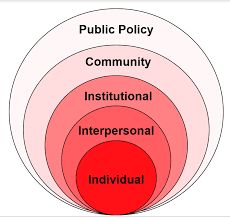
I spoke to using the model to inform a health promotion project on sexually transmitted infections prevention as a tangible way to work through the layers of the social ecological model. Next, a unit focused on chronic diseases and their management and ideally prevention and an opportunity to look at another province’s health system model geared to prevent and treat chronic diseases. I worked with Tanya to compare British Columbia’s approach to that of my home province of Ontario. This was a great exercise and acted as a keen reminder that we are all working within different systems across the country despite existing under Federal ‘Universal’ health care.
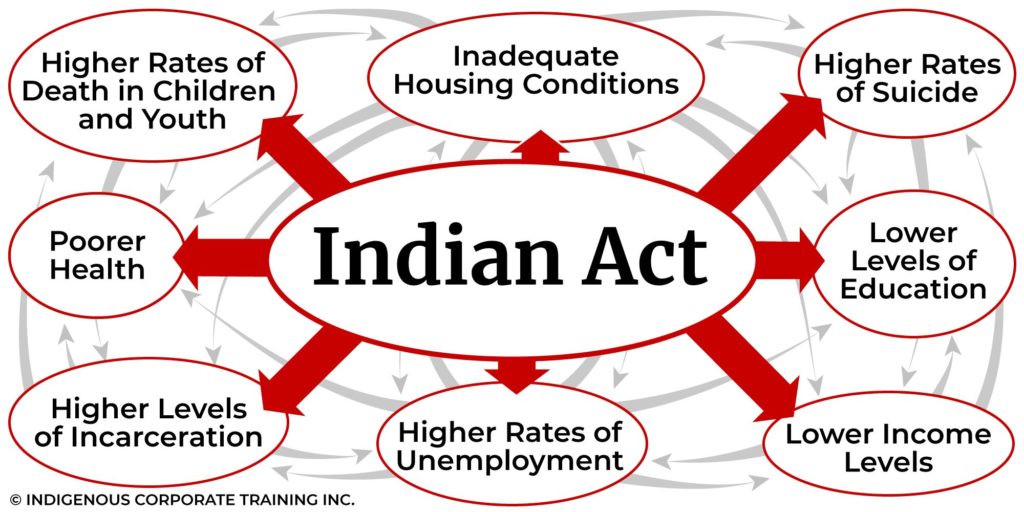
Vulnerable populations were the topic of Unit 6 and it was sobering to further dig into the health disparities that exist in our country currently. The health outcomes of our Indigenous populations are significantly worse than other groups. The life expectancy rates of Indigenous peoples in Canada are lower than that of non-Indigenous peoples in Canada for both men and women by as much as 15 years in some population groups (Public Health Agency of Canada, 2017).
Indigenous people in Canada experience increased rates of type 2 diabetes, hypertension, substance-use disorder, and mental health challenges. Indigenous people in Canada tend to live in more rural regions, have lower rates of educational attainment, and are more likely to live in intergenerational housing and face housing insecurity than non-Indigenous Canadians (Hu & Hajizadeh, 2023). This is just the tip of the injustice iceberg for Canada’s Indigenous populations. Intergenerational trauma, forced assimilation and loss of culture have left deep scars and there is still a very long way to go to begin true reconciliation.
Finally we looked at what is next for health care in Canada (and abroad). COVID-19 is a stark reminder that we are all one world when it comes to health and what affects some of us affects all of us. I am particularly intrigued by AI and the impact it will have on health. I see some tremendous opportunities in improving systems approaches and in evaluating with the intent to improve. #MHST601 has been a great stepping stone into my MHS journey and has set the stage for further learning.
References:
Hu, M., & Hajizadeh, M. (2023). Mind the Gap: What Factors Determine the Worse Health Status of Indigenous Women Relative to Men Living Off-Reserve in Canada?. Journal of racial and ethnic health disparities, 10(3), 1138–1164. https://doi.org/10.1007/s40615-022-01301-x
Med School Insiders. 4 Ways Artificial Intelligence is Transforming Healthcare.
VIDEO: https://youtu.be/TfkHrvct1hg
Durand-Moreau, Q, LaFontaine, J, Ward, Jennifer (2022). Work and health challenges of Indigenous people in Canada. The Lancet, 10(8), E1189-E1197. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(22)00203-0/fulltext
DeCamp, M., DeSalvo, K. & Dzeng, E. (2020). Ethics and Spheres of Influence in Addressing Social Determinants of Health. J GEN INTERN MED 35, 2743–2745. https://doi.org/10.1007/s11606-020-05973-1
Ferdosi, M, McDowell, T, Lewchuk, W, Ross, S. (2022). On how Ontario trialed basic income. UNESCO Inclusive Policy Lab. https://en.unesco.org/inclusivepolicylab/analytics/how-ontario-trialed-basic-income
Public Health Agency of Canada (2017), Health Status of Canadians 2016: Report of the Chief Public Health Officer – How Healthy Are We?, https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/2016-health-status-canadians/page-4-how-healthy-are-we-life-expectancy-birth.html
